Just a reminder, MEQAPI stands for Monitoring & Evaluation, Quality Assurance, and Process Improvement, and you can visit us at http://www.meqapi.org.
Why are we talking about workplace safety?
Firstly, because of the large number of workers and the high rate of injury, the healthcare and social assistance industry has the highest number of injuries of any industry. In the last OSHA report (2010), the healthcare industry reported 653,900 cases of injury (152,000 more than manufacturing). In context, the industry had a non-fatal injury rate of 139.9 per 10,000 workers, compared to the national average of 107.7.
Healthcare workers face a broad array of health risks, ranging from materials they handle and the pathogens they are exposed to, to the patients they see, and even other healthcare workers.
Health care workers face a wide range of hazards on the job, including sharps injuries, harmful exposures to chemicals and hazardous drugs, back injuries, latex allergy, violence, and stress. Although it is possible to prevent or reduce healthcare worker exposure to these hazards, healthcare workers continue to experience injuries and illnesses in the workplace. Cases of nonfatal occupational injury and illness with healthcare workers are among the highest of any industry sector. (CDC-NIOSH)
Occupational Safety and Health Administration (OSHA) expands on this with more specific risks, as follows.
Healthcare workers face a number of serious safety and health hazards. They include bloodborne pathogens and biological hazards, potential chemical and drug exposures, waste anesthetic gas exposures, respiratory hazards, ergonomic hazards from lifting and repetitive tasks, laser hazards, workplace violence, hazards associated with laboratories, and radioactive material and x-ray hazards. Some of the potential chemical exposures include formaldehyde, used for preservation of specimens for pathology; ethylene oxide, glutaraldehyde, and paracetic acid used for sterilization; and numerous other chemicals used in healthcare laboratories. (OSHA)
Some injuries cluster by role. For example, nursing aides, orderlies, and attendants had the highest rates of musculoskeletal injury, with an injury rate of 249 injuries per 10,000 workers compared to a national average of 34.
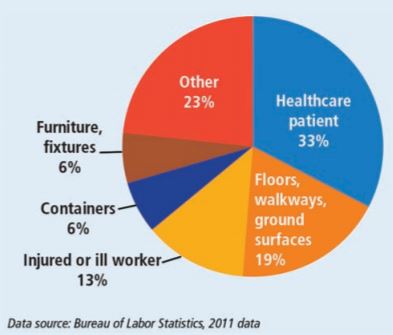
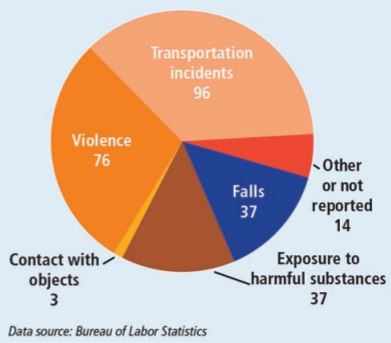
The following graphs were sourced from the OSHA “Facts About Hospital Worker Safety” fact-sheet. From these one can see that sprains, strains, and bruises are the most frequent injury causing days off work. The leading causes were patients, floors, and other workers, with transportation and violence being the most frequent context of injury (with falls and exposure tied in third place).

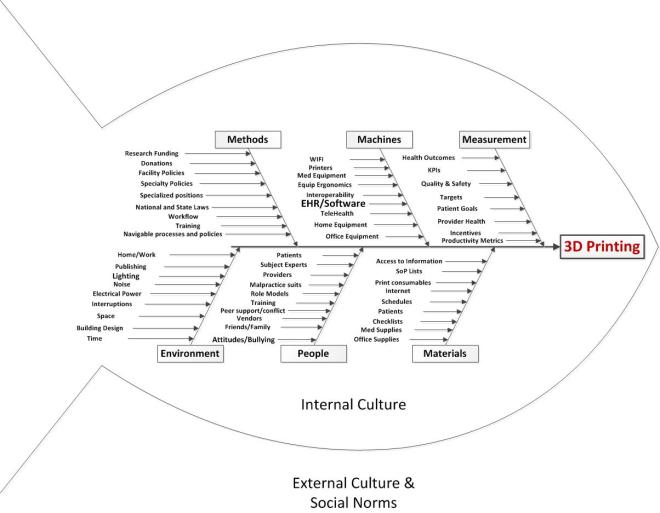
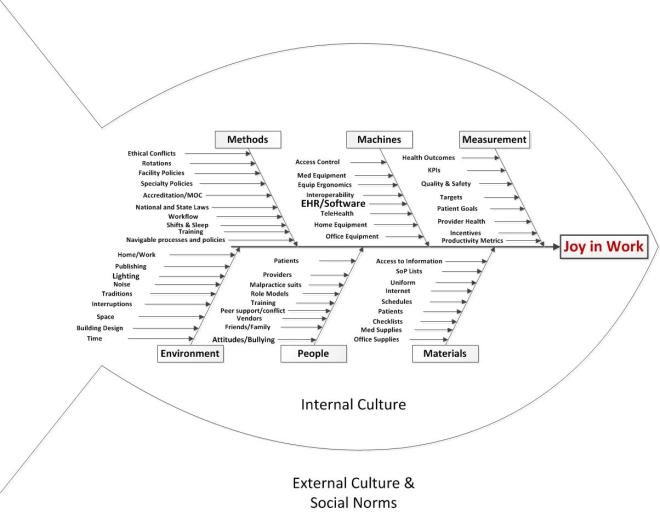
We will take a QI approach, and discuss the topic using each of the typical arms of the basic Quality Improvement Ishikawa diagram to guide and support discussion. An Ishikawa diagram will be provided ahead of time and during the chat.

Participants will bring their own experiences, perspectives, and expectations to the discussion, but the topics might break down something along these lines:
-
- Methods
- Policies: office, organization, or national policies related to workplace safety
- Workflow: how things are done including transportation, care, drug prescription and fulfillment, and laboratory work
- Workload: demands of the job, and whether they exceed the resources and ability to meet the demand.
- Unofficial workarounds
- Safety and quality training
- Quality Improvement and incident reporting policies
- Machines (equipment including EHR)
- Medical or office equipment
- Home equipment specific to the patient condition
- Integration/interoperation with other office or medical systems, or user personal health records
- Medication dispensing systems
- Personal Health Record and encounter planning systems
- Telehealth
- Ergonomics (right size, shape, location, etc)
- WIFI!
- Analytical software
- Incident reporting systems
- People
- Staffing: sufficient and qualified staff
- Training: base training, ongoing training, CME, and patient or carer training
- Attitudes: staff attitudes to technology, adoption vs resistance, bullying
- Fatigue (especially alert fatigue)
- Organizational, specialty, and personal values
- Peer support and role models
- Friends and family
- Unit management
- Materials
- Patients: as the “raw material” of the medical process. Patients may come with a range of attitudes, health problems, life situations, and ability to comply with treatment that are challenging and stressful.
- Supplies: medical or office, inferior fax paper,
- Data: ability to securely share with correct patient, specialist, lab, etc
- Patient self-care materials including checklists and how-to instructions, contact information for questions, and self-care consumables
- Internet sources
- Checklists, SoPs
- Uniforms, footwear, personal protective equipment
- Data!
- Measurement
- Health outcomes
- KPIs: operational metrics required by practice, local government, state, federal
- Quality and safety metrics
- Targets: set by practice, insurer, etc. as well as patient goals
- Incentives and rewards
- Adverse Effects and incident reporting
- Effectiveness of measurement
- Environment
- Noise: distracting noises, sound levels too high, etc. due to computer systems
- Space: Cramped, uncomfortable work space etc.
- Time: Too little time per patient or order, too little time in a day, too many demands
- Location: things where they should be on the screen, click distance, and location of workstation relative to point of care and patient
- Control: the degree to which the individual can control their workload and how to accomplish it
- Fairness: the perception that the burdens and rewards, the effort and outcomes are spread amongst stakeholders in an equitable way
- Interruptions or interference
- Methods
Some of the authors of the works cited above may be responding to the following topics, and participants are invited to describe their experiences of medication errors, and offer their insights and observations.
Topics
- What METHODS enhance or impede workplace safety
- What MACHINE factors enhance or impede workplace safety
- What PEOPLE issues enhance or impede workplace safety
- What MATERIALS enhance or impede workplace safety
- What MEASUREMENT factors enhance or impede workplace safety
- What ENVIRONMENTAL factors enhance or impede workplace safety
Background
MEQAPI focuses on healthcare improvement, and in the spirit of shameless borrowing (and efficiency), takes existing perspectives from the IHI, AHRQ, and others.
To quote the IHI on what the Triple Aim encompasses:
The IHI Triple Aim is a framework developed by the Institute for Healthcare Improvement that describes an approach to optimizing health system performance. It is IHI’s belief that new designs must be developed to simultaneously pursue three dimensions, which we call the “Triple Aim”:
- Improving the patient experience of care (including quality and satisfaction);
- Improving the health of populations; and
- Reducing the per capita cost of health care.
The six domains of care quality (STEEEP) mapped out by the Agency for Healthcare Research and Quality (AHRQ) are foundational to healthcare improvement. All care, and by inference quality measures, should be focused on being Safe, Timely, Effective, Efficient, Equitable, and Patient Centered.
The MEQAPI tweetchat aims to give voice to a broad range of stakeholders in healthcare improvement, and it embraces everyone from administrators to zoologists, and includes physicians, nurses, researchers, bed czars, cleaners, and yes, patients and care-givers.