Topic: Quality Improvement vs EHR Success Story with James Legan MD
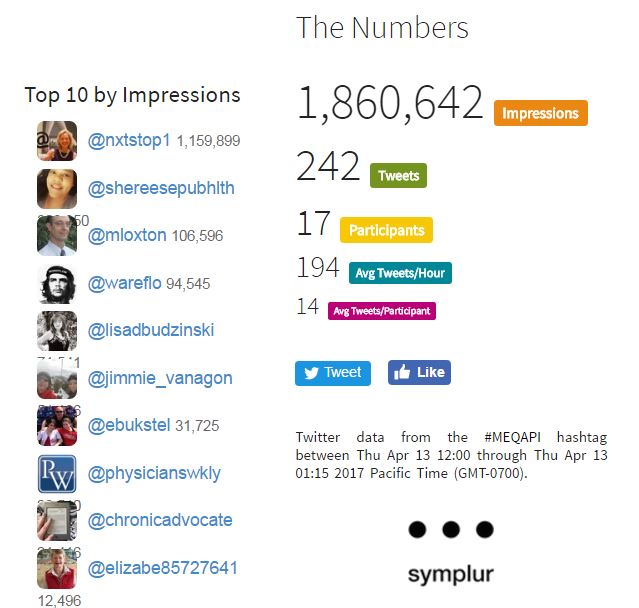
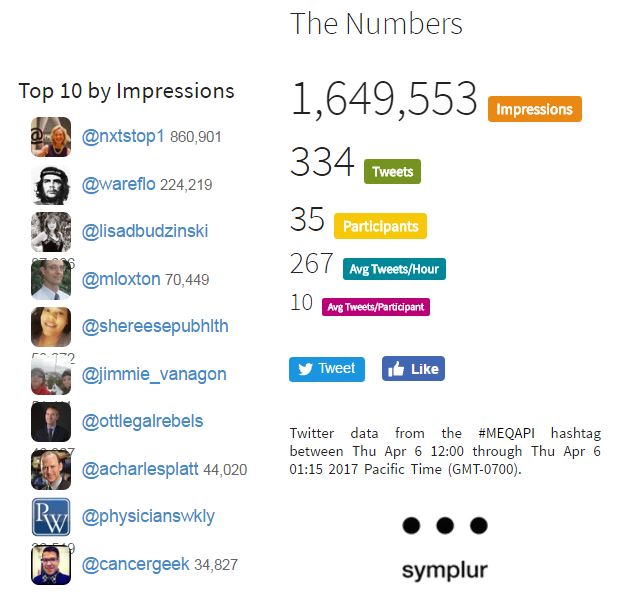
Just a reminder, MEQAPI stands for Monitoring & Evaluation, Quality Assurance, and Process Improvement.
This chat is about using an EHR to improve practice and patient experience.
The HITECH, ARRA, and Meaningful Use programs greatly accelerated adoption of electronic health record (EHR) systems by providers. Adoption by office-based providers rose from 21% in 2004, to 87% by 2015. Many will, however, say that the cost was too high, the results too poor, and that it has potentially soured an entire generation of providers to the idea of Health IT solutions in general and EHR in specific.
While this may be true, there is considerable variation in outcomes and realized value, and wherever there is variation, there is opportunity for quality improvement. For some, the EHR is a frustrating waste of time that is added to an already cramped schedule, and represents an additional burden of several hours of duplicitous administrative work at the end of each workday. For many, the EHR is just another administrative chore. For a few, the EHR has reduced administrative work, improved efficiency, and supportedthe ability to serve patients.
This week the #MEQAPI topics relate to a specific healthcare provider’s experience that may be seen as a positive outlier. Dr. Legan has put together a solution that pairs an EHR and a CRM, and has seen improvements that many would envy. Dr. Legan is an Internal Medicine Physician, in his 23rd year in Private Practice in Great Falls, Montana.Great Falls is in the North Central Montana region, and has approximately 50,000 population, served by two large multi-specialty hospitals. The practice is outpatient-only, and consists of eight physicians: three Internists, four Family Practice, and one Pediatrician, each with approximately 1,200-2,000 patients. Ancillary staff includes five shared in-house billing staff, and each physician has one to three additional support staff.
Dr. Legan has a patient-facing display so that the patient sees everything in the EHR as it is being reviewed or entered.

Dr. Legan describes his outlook on EHR as follows:
I am convinced the electronic health record (EHR) needs to be shared as a visual interactive medium at the point of care. The primary role of the EHR should be educational, all other uses secondary. I discuss this approach #ProjectedEHR on twitter.
Videos of #ProjectedEHR I Periscoped to You Tube
- https://www.youtube.com/watch?v=moTXADdpHtU (me being interviewed)
- https://www.youtube.com/watch?v=HOlKbl1dAWE(interviewing a patient)
- https://www.youtube.com/watch?v=EA5X_LP5_PQ (Wall mounted TV/chromebook)
- https://www.youtube.com/watch?v=kz9rVtRpuI0 (Dual monitored desktop/chromebook in office carried to exam room)
#ProjectedEHR–User friendly EHR that projects well, 14 inch Chromebook, 24 inch TV, 10 foot HDMI cord, 8 inch HDMI extender, wall mount, remote access application made for chrome & encrypted (VNC viewer made for Chrome, Enterprise Version). The chromebook simulates my dual monitored desktop, so I take my “virtual desktop” into the exam room and plug in the HDMI cord to extender and the learning begins. Always check with your IT support to make sure everything is HIPAA compliant and secure.
Some supporting reading for the chat comes from Physician’s Weekly:
- There Is No Such Thing as Too Much TV in This Doctor’s Office: A Different Approach to Patient Engagement
- EHRs: Pros & Cons – Infographic
- Examining EHR Use Among Allergists & Immunologists
- A Q&A on EHRs & MI Care
- EHR Meaningful Use by Specialty
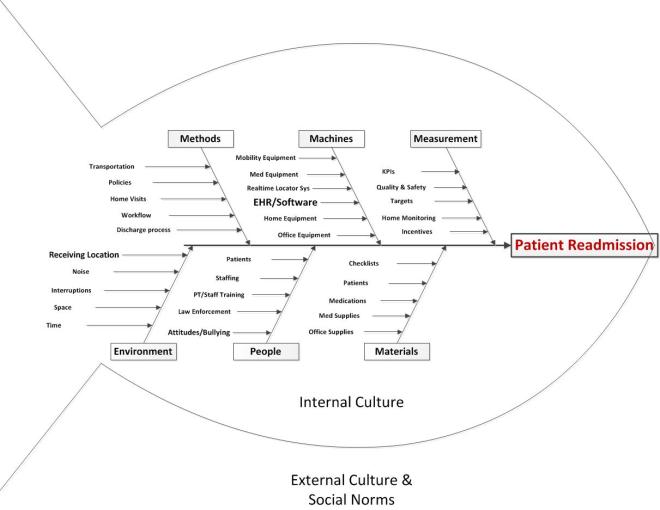
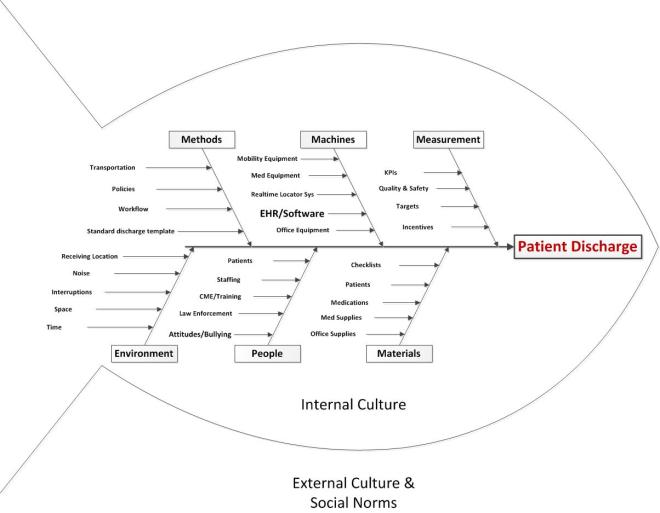
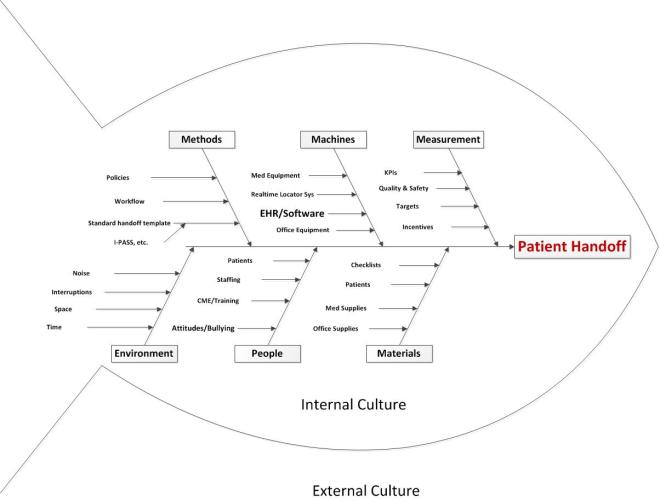
We will take a QI approach, and discuss the topic using each of the typical arms of the basic Quality Improvement Ishikawa diagram to guide and support discussion. An Ishikawa diagram will be provided ahead of time and during the chat.
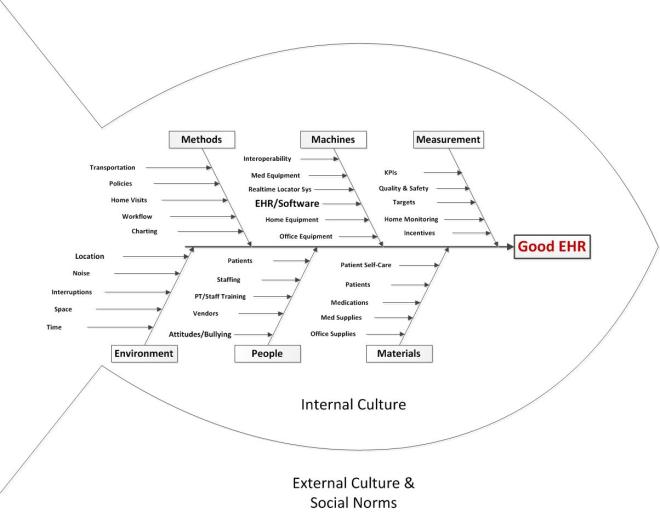
Participants will bring their own experiences, perspectives, and expectations to the discussion, but the topics might break down something along these lines:
-
- Methods
- Policies: office, organization, or national policies, including MU, HIPAA, etc
- Workflow: how things are done including new patient onboarding, care provision, care coordination, ordering/prescribing, billing, patient transfer, etc.
- Insurance Models, payer systems
- Home visits
- Charting – automatic vs manual
- Machines (equipment, EHR)
- Medical or office equipment
- Home equipment specific to the patient condition
- Integration/interoperation with other office or medical systems, or user personal health records
- People
- Staffing: sufficient and qualified staff
- Training: base training, ongoing training, CME, and patient or carer training
- Attitudes: staff attitudes to technology, adoption vs resistance
- Materials
- Patients: as the “raw material” of the medical process. Patients may come with a range of attitudes, health problems, life situations, and ability to comply with treatment that are challenging and stressful.
- Supplies: medical or office, inferior fax paper,
- Data: ability to securely share with correct patient, specialist, lab, etc
- Patient self-care materials including checklists and how-to instructions, contact information for questions, and self-care consumables
- Measurement
- KPIs: operational metrics required by practice, local government, state, federal
- Quality and safety metrics
- Targets: set by practice, insurer, etc.
- Monitoring of home-care
- Environment
- Noise: distracting noises, sound levels too high, etc. due to computer systems
- Space: ergonomic requirements of system- maybe leading to cramped, uncomfortable work space etc.
- Time: Too little time per patient, too little time in a day, too many demands
- Location: things where they should be on the screen, click distance, and location of workstation relative to point of care and patient
- Methods
Dr. Legan will be responding to the following topics with regard to his own system, and will field questions from other participants. Participants are also invited to respond with regard to their experiences of EHRs, and offer their insights and observations.
Topics
- What risks, issues, opportunities, or observations did you have related to Methods and your EHR/CRM solution
- What risks, issues, opportunities, or observations did you have related to Machines and your EHR/CRM solution
- What risks, issues, opportunities, or observations did you have related to People issues and your EHR/CRM solution
- What risks, issues, opportunities, or observations did you have related to Materials and your EHR/CRM solution
- What risks, issues, opportunities, or observations did you have related to Measurements and your EHR/CRM solution
- What risks, issues, opportunities, or observations did you have related to Environment issues and your EHR/CRM solution
Background
MEQAPI focuses on healthcare improvement, and in the spirit of shameless borrowing (and efficiency), takes existing perspectives from the IHI, AHRQ, and others.
To quote the IHI on what the Triple Aim encompasses:
The IHI Triple Aim is a framework developed by the Institute for Healthcare Improvement that describes an approach to optimizing health system performance. It is IHI’s belief that new designs must be developed to simultaneously pursue three dimensions, which we call the “Triple Aim”:
- Improving the patient experience of care (including quality and satisfaction);
- Improving the health of populations; and
- Reducing the per capita cost of health care.
The six domains of care quality (STEEEP) mapped out by the Agency for Healthcare Research and Quality (AHRQ) are foundational to healthcare improvement. All care, and by inference quality measures, should be focused on being Safe, Timely, Effective, Efficient, Equitable, and Patient Centered.
The MEQAPI tweetchat aims to give voice to a broad range of stakeholders in healthcare improvement, and it embraces everyone from administrators to zoologists, and includes physicians, nurses, researchers, bed czars, cleaners, and yes, patients and care-givers.