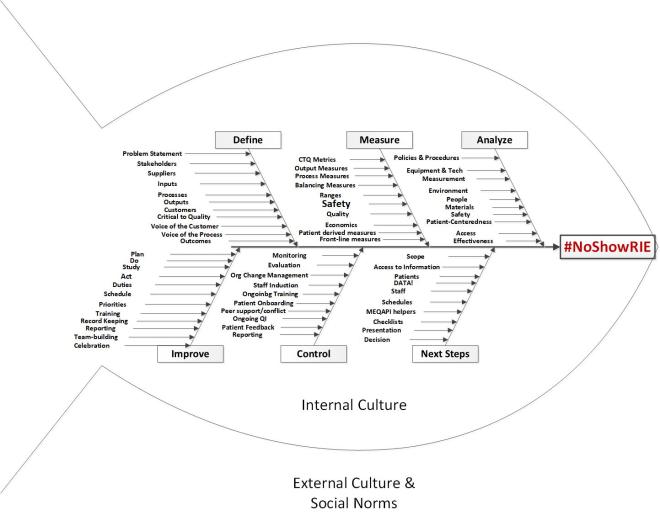
Just a reminder, MEQAPI stands for Monitoring & Evaluation, Quality Assurance, and Process Improvement, and you can visit us at http://www.meqapi.org
We have written before that “Patient voice” is a critical component of quality improvement (QI) and has been a neglected area in healthcare. While clinicians and healthcare workers strive to be patient-centered and to do their best for patients, this does not often manifest in including patients when it comes to planning changes, making decisions, or developing policies. As a result, patients are often a neglected voice in healthcare improvement, even when they are the central goal.
As we describe in a Physician’s Weekly blog “Micro-Study: Discovering the Patient Voice“, we are conducting a study into how patients and care-givers experience radiology:
This micro research project seeks to understand key experiences of the patient’s journey. The project will focus on the radiology care pathway, and the patient journey through the end-to-end experience, from initial encounter that decided on a radiological service, to the final discussion of findings, and billing for radiology services. One aspect the study will seek to illuminate is the opportunity to establish patient reported outcomes (PRO) measurements. PRO metrics will be a BIG DEAL in improving the care experience and reducing medical mistakes.
In their British Medical Journal (BMJ) paper titled “What can patients tell us about the quality and safety of hospital care? Findings from a UK multicentre survey study“, O’Hara et al discuss a study of patient experience of safety. The study analyzed data from 2,471 patients across 33 wards in three English NHS Trusts, between May 2013 and September 2014.
O’Hara et al found a high rate of patient-reported incidents, but perhaps the most eye-opening finding was that 10% of the patients identified a patient safety issue (boldface added)
Of the 2471 inpatients recruited, 579 provided 1155 patient-reported incident reports. 14 categories were developed for classification of reports, with communication the most frequently occurring (22%), followed by staffing issues (13%) and problems with the care environment (12%). 406 of the total 1155 patient incident reports (35%) were classified by clinicians as a patient safety incident according to the standard definition. 1 in 10 patients (264 patients) identified a patient safety incident, with medication errors the most frequently reported incident.
To put this number into perspective, CDC figures for 2015, show that 83.6% of the U.S. adult population had at least one healthcare encounter in the preceding year, translating into 125.7 million hospital visits, and 990.8 million physician office visits. If 10% of patients discovered and reported a safety issue in that year, millions of additional opportunities for improvement would result.
Some additional sources for this chat:
- Can patient involvement improve patient safety? A cluster randomised control trial of the Patient Reporting and Action for a Safe Environment (PRASE) intervention
- How might health services capture patient-reported safety concerns in a hospital setting? An exploratory pilot study of three mechanisms
- The patient reporting and action for a safe environment (PRASE) intervention: a feasibility study
- Exploring how ward staff engage with the implementation of a patient safety intervention: a UK-based qualitative process evaluation
- The Patient Feedback Response Framework – Understanding why UK hospital staff find it difficult to make improvements based on patient feedback: A qualitative study
Topics
- In your experience with radiology as a patient or care-giver, can you recall something that surprised you?
– What was it?
– What part of the radiological process did it relate to? E.g. getting an x-ray, booking an appointment, filling in the forms, etc.
– How did this affect you? i.e did something bad happen, like missing an appointment, etc. - In your experience with radiology as a patient or care-giver, can you recall something that confused you?
– What was it?
– What part of the radiological process did it relate to? E.g. getting an x-ray, booking an appointment, filling in the forms, etc.
– How did this affect you? i.e did something bad happen, like missing an appointment, etc. - In your experience with radiology as a patient or care-giver, can you recall something that frustrated you?
– What was it?
– What part of the radiological process did it relate to? E.g. getting an x-ray, booking an appointment, filling in the forms, etc.– How did this affect you? i.e did something bad happen, like missing an appointment, etc.
- Looking over the entire experience, what parts did you feel worked well for you – anything from the way appointments were booked or parking was set out to how the scan or procedure was done
- What parts did you feel worked poorly for you – again, could be anything from the way appointments were booked or parking was set out to how the scan or procedure was done
- What one thing (or two) would you say radiologists need to improve, and what would that look like?
Background
MEQAPI focuses on healthcare improvement, and in the spirit of shameless borrowing (and efficiency), takes existing perspectives from the IHI, AHRQ, and others.
To quote the IHI on what the Triple Aim encompasses:
The IHI Triple Aim is a framework developed by the Institute for Healthcare Improvement that describes an approach to optimizing health system performance. It is IHI’s belief that new designs must be developed to simultaneously pursue three dimensions, which we call the “Triple Aim”:
- Improving the patient experience of care (including quality and satisfaction);
- Improving the health of populations; and
- Reducing the per capita cost of health care.
The six domains of care quality (STEEEP) mapped out by the Agency for Healthcare Research and Quality (AHRQ) are foundational to healthcare improvement. All care, and by inference quality measures, should be focused on being Safe, Timely, Effective, Efficient, Equitable, and Patient Centered. We expand this to include Affordability, STEEEPA.
The MEQAPI tweetchat aims to give voice to a broad range of stakeholders in healthcare improvement, and it embraces everyone from administrators to zoologists, and includes physicians, nurses, researchers, bed czars, cleaners, and yes, patients and care-givers.
The Author and Moderator: Matthew is a principal analyst for healthcare improvement at the Washington D.C. based firm of Whitney, Bradley, and Brown (WBB), and is a strategic adviser and board member at the Blue Faery Liver Cancer Association. Matthew is a peer reviewer for the international journal of Knowledge Management Research and Practice, and blogs regularly for Physician’s Weekly.